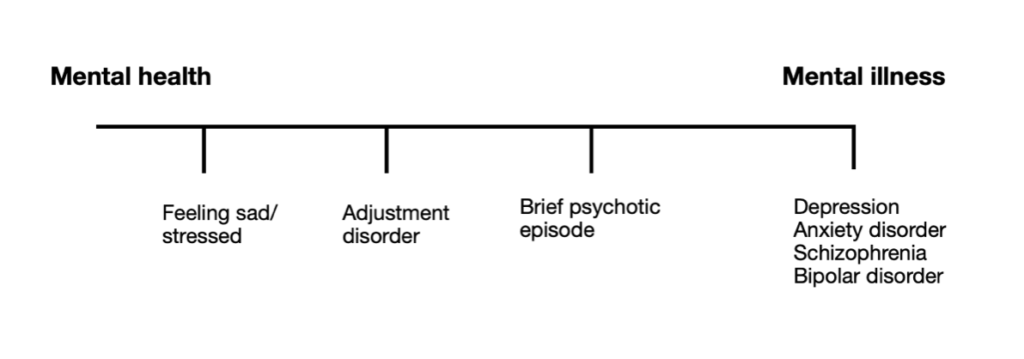
Mental health exists on a spectrum. At different times in our lives we may sit at different points along it — from feeling well and resilient to experiencing distress, depression, or even a loss of contact with reality. Understanding this spectrum helps us respond with the right mix of self-care, therapy, and medical treatment when needed.
The Mental Health Spectrum in Everyday Life
Mental health is an essential feature of being human. Over the last century, our understanding has deepened from simple ideas about “nerves” or “melancholy” to a far more nuanced awareness that mental wellbeing exists on a continuum. It spans everyday foundations — sleep, nutrition, movement, connection — through to complex, lifelong illnesses such as bipolar disorder and schizophrenia, which are strongly influenced by genetic and biological factors.
Greater visibility in the media and workplaces has helped to destigmatise conversation and encourage earlier help-seeking. At the same time, not all challenges can be solved by lifestyle changes alone. Some mental illnesses arise through no fault of our own and may require ongoing medical care — just as diabetes or epilepsy do.
Ready to talk to a therapist?
Confidential, compassionate support — online or in person. If you’re unsure where you sit on the mental health spectrum, a guided assessment can help.
Book an AppointmentWhen Stress Tips Into an Adjustment Disorder
As life stress builds — relationship changes, job loss, illness or bereavement — we might move along the spectrum into low mood, worry, or exhaustion. For many, these experiences are part of being human and can improve with self-care, time and support. Sometimes, however, distress becomes an Adjustment Disorder with symptoms that resemble depression: sadness, anxiety, difficulty concentrating, disrupted sleep, and loss of interest. With care and space to adapt, most people recover.
When Depression Becomes an Illness
Sometimes a low mood doesn’t lift. Brain chemistry can shift and symptoms deepen and persist. This may become a Major Depressive Episode — where hopelessness, worthlessness, and loss of pleasure take hold. Antidepressant medication and psychological therapy are often effective partners: medication can restore balance so therapy and lifestyle strategies can work better. Depression takes many forms — reactive to events, part of bipolar disorder, or without a clear trigger — and each deserves assessment and tailored treatment.
When Reality Feels Out of Reach
At the far end of the spectrum are psychotic illnesses such as schizophrenia, schizoaffective disorder and severe bipolar disorder. During a psychotic episode, a person may experience delusions (fixed false beliefs) or hallucinations (hearing or seeing things others don’t). Insight is often lost, so reasoning with the person rarely helps. Medical treatment is vital: antipsychotic medications can reduce symptoms, restore insight, and help people reconnect with reality. Some short-lived, reactive psychoses occur after extreme stress and can resolve fully with treatment and support; others require ongoing care.
Compassion, Not Blame
One of the most harmful myths is that people should “snap out of it.” We don’t blame someone for needing insulin; we shouldn’t blame someone for needing therapy or medication. Mental health care is about kindness and practicality: matching the right support to the person’s needs so they can live a meaningful life. Meanwhile, simple habits — sleep, movement, nature time, mindfulness, social connection — can protect and strengthen wellbeing for all of us.
A Shared Human Experience
Mental health is not something that only “some people” struggle with. Every one of us moves along the mental health spectrum at different times. When society talks openly about the full range — from everyday stress to serious illness — stigma dissolves and people get help sooner.
FAQs
What does “mental health spectrum” actually mean?
It’s the idea that mental health is not binary. Our wellbeing shifts over time, from feeling balanced and resilient to experiencing distress or illness. Recognising the spectrum helps us choose the right support — from self-care to therapy and medical treatment.
How do I know if I need therapy, medication, or both?
If low mood, anxiety, or sleep issues persist beyond a few weeks or impact work, study, or relationships, it’s worth seeking a professional assessment. Many people benefit from therapy alone; others improve fastest with a combination of therapy and medication.
Can lifestyle changes cure serious mental illness?
Healthy habits support recovery but generally can’t replace medical treatment for conditions like major depression, bipolar disorder, or schizophrenia. These illnesses are biological in nature and respond best to medication and sophisticated medical care.
What should I do if a loved one seems out of touch with reality?
Stay calm, avoid arguing about beliefs, ensure safety, for yourself and loved one, and seek urgent professional help. Early treatment during a first episode of psychosis can improve outcomes significantly.

